Intraventricular Hemorrhage
| Other | Intraventricular Hemorrhage |
| Names | Intraventricular Bleeding |
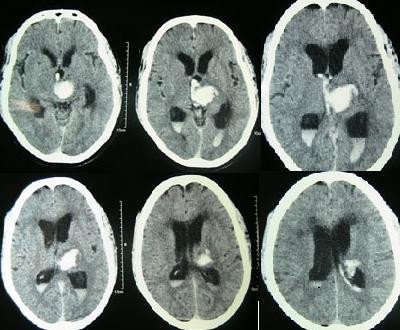
CT scan showing spontaneous intracerebral hemorrhage with bleeding in the third and both lateral ventricles and hydrocephalus[1]
Intraventricular hemorrhage (IVH), also known as intraventricular bleeding, is a bleeding into the brain's ventricular system, where the cerebrospinal fluidis produced and circulates through towards the subarachnoid space. It can result from physical trauma or from hemorrhaging in stroke.
30% of intraventricular hemorrhage (IVH) are primary, confined to the ventricular system and typically caused by intraventricular trauma, aneurysm, vascular malformations, or tumors, particularly of the choroid plexus. [2] However 70% of IVH are secondary in nature, resulting from an expansion of an existing intraparenchymal or subarachnoid hemorrhage. [2] Intraventricular hemorrhage has been found to occur in 35% of moderate to severe traumatic brain injuries. [3]Thus the hemorrhage usually does not occur without extensive associated damage, and so the outcome is rarely good. [4][5]
Contents
Symptoms and Diagnosis
Symptoms of IVH are similar to other intracerebral hemorrhages and include sudden onset of headache, nausea and vomiting, together with an alteration of the mental state and/or level of consciousness.[6] Focal neurological signs are either minimal or absent, but focal and/or generalized seizures may occur.[6] Xanthochromia, yellow-tinged CSF, is the rule.[6] Diagnosis can be confirmed by the presence of blood inside the ventricles on CT.
Associated Conditions
Brain contusions and subarachnoid hemorrhages are commonly associated with IVH.[7] The bleeding can involve the anterior communicating artery or the posterior communicating artery. In both adults and infants, IVH can cause dangerous increases in ICP, damage to the brain tissue, and hydrocephalus.[8][9]
Treatment
Treatment focuses on monitoring and should be accomplished with inpatient floor service for individuals responsive to commands or neurological ICU observation for those with impaired levels of consciousness.[10] Extra attention should be placed on intracranial pressure (ICP) monitoring via an intraventricular catheter and medications to maintain ICP, blood pressure, and coagulation.[2]In more severe cases an external ventricular drain may be required to maintain ICP and evacuate the hemorrhage, and in extreme cases an open craniotomy may be required.[2][10] In cases of unilateral IVH with small intraparenchymal hemorrhage the combined method of stereotaxy and open craniotomy has produced promising results. [11]
Prognosis
Prognosis is also very poor when IVH results from intracerebral hemorrhage related to high blood pressure and is even worse when hydrocephalus follows.[1] It can result in dangerous increases in ICP and can cause potentially fatal brain herniation. [1] Even independently, IVH can cause morbidity and mortality. First, intraventricular blood can lead to a clot in the CSF conduits blocking its flow and leading to obstructive hydrocephalus which may quickly result in increased intracranial pressure and death.[10] Second, the breakdown products from the blood clot may generate an inflammatory response that damages the arachnoid granulations, inhibiting the regular reabsorption of CSF and resulting in permanent communicating hydrocephalus. [2][10]
Babies
IVH in the preterm brain usually arises from the germinal matrix whereas IVH in the term infants originates from the choroid plexus. However, it is particularly common in premature infants or those of very low birth weight. [8]The cause of IVH in premature infants, unlike that in older infants, children or adults, is rarely due to trauma. Instead it is thought to result from changes in perfusion of the delicate cellular structures that are present in the growing brain, augmented by the immaturity of the cerebral circulatory system, which is especially vulnerable to hypoxic ischemic encephalopathy . The lack of blood flow results in cell death and subsequent breakdown of the blood vessel walls, leading to bleeding. While this bleeding can result in further injury, it is itself a marker for injury that has already occurred. Most intraventricular hemorrhages occur in the first 72 hours after birth.[8]The risk is increased with use of extracorporeal membrane oxygenation in preterm infants.[12] Congenital cytomegalovirus infection can be an important cause.[13]
The amount of bleeding varies. IVH is often described in four grades:
- Grade I - bleeding occurs just in the germinal matrix
- Grade II - bleeding also occurs inside the ventricles, but they are not enlarged
- Grade III - ventricles are enlarged by the accumulated blood
- Grade IV - bleeding extends into the brain tissue around the ventricles
Grades I and II are most common, and often there are no further complications. Grades III and IV are the most serious and may result in long-term brain injury to the infant. After a grade III or IV IVH, blood clots may form which can block the flow of cerebrospinal fluid, leading to increased fluid in the brain (hydrocephalus).
There have been various therapies employed into preventing the high rates of morbidity and mortality, including diuretic therapy,[14] repeated lumbar puncture,[15] streptokinase therapy [16] and most recently combination a novel intervention called DRIFT (drainage, irrigation and fibrinolytic therapy).
In 2002, a Dutch retrospective study[17] analysed cases where neonatologists had intervened and drained CSF by lumbar or ventricular punctures if ventricular width (as shown on ultrasound) exceeded the 97th centile as opposed to the 97th centile plus 4 mm.[18] Professors Whitelaw's original Cochrane review[14] published in 2001 as well as evidence from previous randomised control trials indicated that interventions should be based on clinical signs and symptoms of ventricular dilatation. An international trial has instead looked an early (97th centile) versus late (97th centile plus 4 mm) for intervening and draining CSF.[19]
DRIFT has been tested in an international randomised clinical trial; although it did not significantly lower the need for shunt surgery, severe cognitive disability at two years Bayley (MDI <55) was significantly reduced.[20] Repeated lumbar punctures are used widely to reduce the effects in increased intracranial pressure and an alternative to ventriculoperitoneal (VP) shunt surgery that cannot be performed in case of intraventricular haemorrhage. The relative risk of repeated lumbar puncture is close to 1.0, therefore it is not statistically therapeutic when compared to conservative management and does raise the risk of subsequent CSF infection.[15]